It was 2014 when Alliance adopted an organizational vision to be a leader in transforming the delivery of whole person care in North Carolina’s public sector, and we have been working towards the fulfillment of that vision ever since. Early on, we were strong advocates for a model of care delivery that not only integrates the physical, behavioral and pharmacy care of our health plan participants, but also addresses the social and environmental factors that are critically impactful on their well-being.
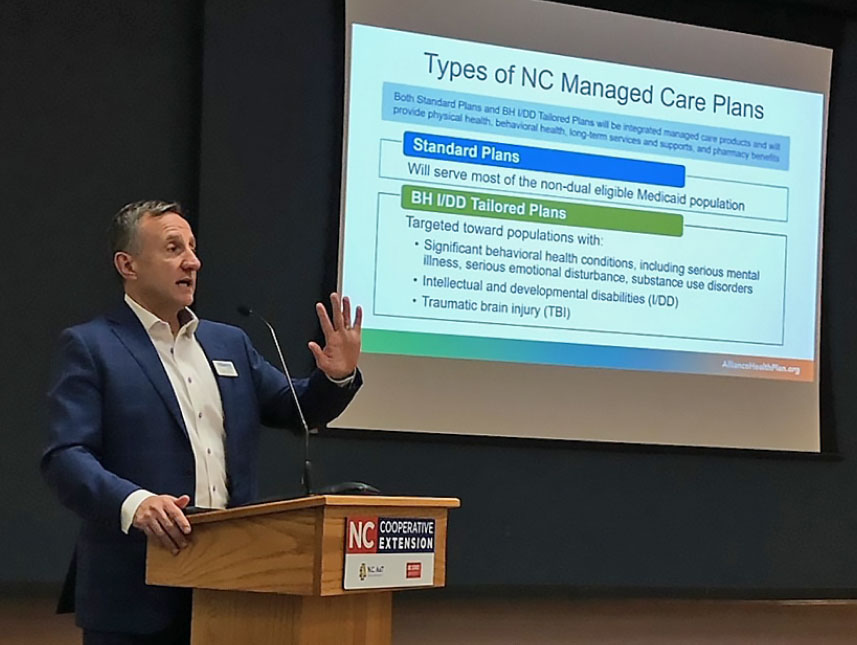
This year, our preparations for Tailored Plan operations continued and even accelerated to reflect Alliance’s critical role in our state’s most ambitious transformation of its public health care system to date. We grew our comprehensive network of providers by 683, including 628 primary care practices, medical specialists, hospital systems, community health centers, laboratories and skilled nursing facilities, helping ensure that our participants can retain their current physical health care providers in 2023 under our Tailored Plan. We’re also working to build a robust roster of member pharmacies to meet network adequacy standards.
Our work in 2022 reaffirmed our commitment to the health and well-being of vulnerable children and youth and their families. In this report we’ll tell you about an exciting new child behavioral health urgent care and facility-based crisis center that is on the horizon, as well as other new programs that provide stabilization and assessment services to young people experiencing a crisis. We’ll also update you on Alliance’s award-winning school-based program that provides system coordination when a child is experiencing a crisis or is in transition to and from crisis or residential placements such as psychiatric residential treatment facilities.
We’ll highlight Alliance’s successful launch of Tailored Care Management, providing community-based, provider-driven care to improve whole- person care and health outcomes for the people we serve.
You’ll read about our efforts across our region, often involving local partnerships, designed to expand treatment capacity and increase access to community-based behavioral health services and crisis response so people can quickly receive the treatment they need before more restrictive and costly interventions become necessary.
At Alliance, we consider safe, stable housing to be a health care intervention, and we’ll detail our latest additions to an already robust inventory of housing assistance, including our investment in an innovative tiny home project.
As always, our Alliance team of exceptional professionals – 957 at year’s end, representing 23% growth during 2022 – has focused daily on enhancing and managing innovative, evidenced-based services and supports that allow members of our health plan to live healthier, more satisfying lives.
Our work is enhanced by the guidance of an outstanding board of directors, as well as the support of the boards of county commissioners and the county managers and their staffs from our six counties. We thank them all, along with our Consumer and Family Advisory Committee and our partners and colleagues across the Alliance region.